Exercise is one of the most effective tools for managing diabetes. It improves insulin sensitivity, lowers blood sugar, and enhances overall health. For people with diabetes, staying active helps control blood glucose levels, reduces complications, and improves quality of life. Whether you have Type 1, Type 2, or prediabetes, understanding how to safely exercise is key to making it a part of your diabetes management plan.

The Impact of Exercise on Diabetes
Exercise has a direct impact on your blood glucose levels, making it an essential part of diabetes care. When you work out, your muscles use glucose (sugar) as fuel. This helps lower blood glucose levels both during and after exercise. Over time, regular physical activity increases your insulin sensitivity, allowing your body to use insulin more effectively.
Here are some of the key ways exercise benefits people with diabetes:
1. Improved Blood Glucose Control:
– Studies show that exercise lowers blood sugar levels immediately and improves overall glycemic control over time. According to research published in *Diabetes Care*, both aerobic and resistance exercises reduce HbA1c (a measure of long-term blood sugar control) levels in people with Type 2 diabetes (Colberg et al., 2010).
2. Enhanced Insulin Sensitivity:
– Physical activity increases the body’s sensitivity to insulin, making it easier for cells to absorb glucose from the bloodstream. This reduces the need for insulin or medication and helps prevent insulin resistance.
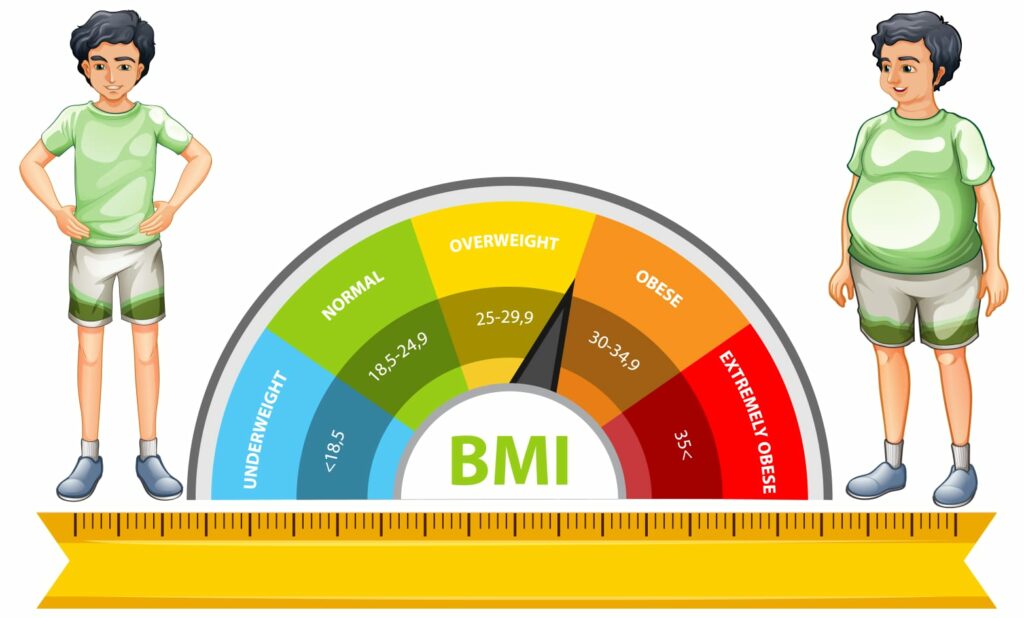
3. Weight Management:
– Exercise helps burn calories and promotes fat loss, which is especially important for people with Type 2 diabetes, where excess weight can worsen insulin resistance. Regular exercise also helps preserve muscle mass while losing fat.
4. Reduced Risk of Complications:
– Regular exercise lowers the risk of cardiovascular disease, one of the most common complications of diabetes. It helps reduce blood pressure, improve cholesterol levels, and enhance overall heart health.
5. Mental Health Benefits:
– Living with diabetes can be stressful, but exercise helps reduce anxiety, depression, and improve mood by releasing endorphins. Regular physical activity is linked to better mental health and well-being.
Best Exercises for Managing Diabetes
When it comes to diabetes, the type of exercise you choose is important. A balanced routine that includes aerobic, strength, and flexibility exercises works best for managing diabetes.
1. Aerobic Exercise
– Aerobic activities, such as walking, swimming, cycling, and dancing, increase heart rate and improve circulation, which helps manage blood sugar levels. Aim for at least 150 minutes of moderate-intensity aerobic activity per week, as recommended by the American Diabetes Association (ADA).
– Walking is one of the best options for beginners. It’s low-impact, accessible, and highly effective for controlling blood sugar levels.

2. Resistance Training
– Strength training exercises (like lifting weights or using resistance bands) build muscle and help the body absorb glucose more effectively. Muscle tissue burns more glucose than fat, even at rest, making resistance training essential for long-term diabetes management.
– According to a study in Diabetes Care, resistance training, performed two to three times per week, significantly improves glycemic control and insulin sensitivity in people with Type 2 diabetes (Ibañez et al., 2005).

3. High-Intensity Interval Training (HIIT)
– HIIT involves alternating short bursts of intense exercise with periods of rest or lower intensity. This form of exercise improves cardiovascular fitness and helps lower blood sugar more effectively than moderate-intensity exercise alone. Research in the Journal of Diabetes Research suggests that HIIT improves glycemic control and insulin sensitivity in people with Type 2 diabetes (Gillen & Gibala, 2014).

4. Flexibility and Balance Training
– Exercises like yoga, Pilates, and tai chi improve flexibility, balance, and strength while promoting relaxation and reducing stress. Studies show that these exercises can also help improve blood sugar control and lower stress hormones, which can have an indirect effect on blood glucose management.

Safe Exercise Tips for People with Diabetes
While exercise offers many benefits, it’s important to approach it with caution if you have diabetes. Here are some essential tips to help you stay safe while working out:
1. Monitor Blood Sugar Levels:
– Before starting any exercise, always check your blood sugar levels. If it’s below 100 mg/dL, have a small carbohydrate-rich snack to prevent hypoglycemia. If it’s above 250 mg/dL, you may need to postpone exercise until your levels are more stable.
2. Carry a Fast-Acting Carb:
– Hypoglycemia (low blood sugar) is a common concern during exercise, especially if you’re on insulin or medications that lower blood sugar. Always carry fast-acting carbohydrates, like glucose tablets, juice, or candy, in case your blood sugar drops suddenly.
3. Start Slowly:
– If you’re new to exercise or haven’t been active for a while, ease into it. Start with 10-15 minutes of light exercise, like walking, and gradually increase duration and intensity. Sudden, intense exercise can lead to drastic changes in blood sugar levels.
4. Stay Hydrated:
– Dehydration can lead to elevated blood sugar levels, so make sure to drink plenty of water before, during, and after exercise.
5. Check Your Feet:
– People with diabetes are at higher risk for foot injuries due to poor circulation and nerve damage. Always wear comfortable, well-fitting shoes, and check your feet for blisters, cuts, or sores after each workout.
6. Warm Up and Cool Down:
– Start every workout with a 5-10 minute warm-up to gradually increase your heart rate and prepare your muscles. Similarly, end your exercise session with a cool-down period to gradually bring your heart rate back to normal.
7. Consult Your Healthcare Provider:
– Always talk to your healthcare provider before starting a new exercise routine, especially if you have diabetes complications like neuropathy, heart disease, or retinopathy. They can help you determine which exercises are safest for your condition.
8. Avoid Exercising Alone:
– If you’re prone to hypoglycemia, it’s a good idea to exercise with a partner or in a supervised environment. Always inform others about your condition and let them know how to help in case of an emergency.
Conclusion
Exercise is a cornerstone of diabetes management, providing numerous health benefits that go beyond just controlling blood sugar. By combining aerobic activities, strength training, and flexibility exercises, you can improve your blood glucose levels, enhance insulin sensitivity, and lower the risk of complications. However, safety should always come first—monitor your blood sugar, stay hydrated, and consult your healthcare provider before starting any new workout routine.