Ulcerative Colitis
What is Ulcerative Colitis
Ulcerative colitis (UC) is a chronic inflammatory bowel disease characterized by inflammation of the colon and rectum. During periods of remission, when symptoms are under control, nutrition plays a crucial role in maintaining gut health and preventing flare-ups. Crafting a healing diet tailored to individual needs can help manage symptoms and promote overall well-being.
Ulcerative colitis (UC) is primarily classified based on the extent and location of inflammation within the colon and rectum. The main types of ulcerative colitis include:
- Ulcerative Proctitis: In this type, inflammation is limited to the rectum, the lowest part of the colon. This form of UC tends to be milder compared to other types and may not involve systemic symptoms like fatigue or weight loss.
- Proctosigmoiditis: It involves inflammation of the rectum and the sigmoid colon (the lower portion of the colon nearest to the rectum).
- Left-Sided Colitis: In left-sided colitis, inflammation extends from the rectum up to the splenic flexure, which is the bend in the colon near the spleen.
- Pancolitis: Pancolitis, also known as total colitis, involves inflammation of the entire colon, from the rectum to the cecum (the beginning of the colon).
- Acute Severe Ulcerative Colitis (Fulminant Colitis): This is a severe form of UC characterized by intense inflammation and rapid onset of symptoms.
Acute severe ulcerative colitis requires immediate medical attention and may necessitate hospitalization for intensive treatment, including intravenous fluids, corticosteroids, and potentially surgery if medical therapy fails.
Need to consult?
Quickly Book an Appointment.

Symptoms of Ulcerative Colitis
Symptoms can vary in severity and may come and go over time. Common symptoms of ulcerative colitis include:
- Diarrhea: Persistent diarrhea is one of the hallmark symptoms of UC. Stools may be loose, watery, and may contain blood or mucus.
- Abdominal Pain and Cramping: Individuals with UC often experience abdominal discomfort, cramping, and pain, particularly during bowel movements or after eating.
- Rectal Bleeding: Blood in the stool is a common symptom of UC. It may appear bright red or maroon and may be mixed with stool or seen on toilet paper.
- Urgency to Defecate: Many people with UC experience a sudden and urgent need to have a bowel movement, which can be difficult to control.
- Incomplete Bowel Movements: Despite the urgency to defecate, individuals with UC may feel like they haven’t completely emptied their bowels.
- Weight Loss: Chronic inflammation and diarrhea can lead to weight loss and malnutrition in some cases.
- Fatigue: Persistent inflammation and frequent bowel movements can cause fatigue and weakness, even if you’re getting enough rest.
- Fever: Some individuals with UC may experience low-grade fevers during flare-ups, which are episodes of increased disease activity.
- Loss of Appetite: Decreased appetite and feelings of fullness can occur due to inflammation and discomfort in the digestive tract.
- Joint Pain: Inflammation associated with UC can also affect the joints, leading to pain and stiffness, particularly in the knees, wrists, and ankles.
Diagnosis
The diagnosis of ulcerative colitis (UC) typically involves a combination of medical history evaluation, physical examination, laboratory tests, imaging studies, and endoscopic procedures
- Medical History and Physical Examination
- Laboratory Tests:
- Imaging Studies:
- Endoscopic Procedures
- Colonoscopy
Managing Ulcerative Colitis
Crafting a healing diet tailored to individual needs can help manage symptoms and promote overall well-being.
- Low-Residue Diet: During flare-ups or periods of active inflammation, a low-residue diet may help reduce bowel movements and minimize irritation to the digestive tract. This diet limits high-fiber foods such as raw fruits and vegetables, whole grains, nuts, and seeds.
- Soft, Easily Digestible Foods: Opt for softer foods that are easier to digest, such as cooked fruits and vegetables, tender meats, fish, eggs, and well-cooked grains like rice and oats.
- Stay Hydrated: Drink plenty of fluids to stay hydrated, especially if experiencing diarrhea. Water, herbal teas, and clear broths are good options. Avoid carbonated beverages and caffeine, as they may exacerbate symptoms.
- Limit Dairy and Lactose: Some individuals with UC may be lactose intolerant or have difficulty digesting dairy products. Consider limiting or avoiding dairy and lactose-containing foods such as milk, cheese, and ice cream, especially if they worsen symptoms.
- Mindful Eating: Eat smaller, more frequent meals to reduce the workload on the digestive system and minimize discomfort. Chew food thoroughly and eat slowly to aid digestion and prevent gas and bloating.
- Probiotic and Prebiotic Foods: Incorporate probiotic-rich foods like yogurt, kefir, sauerkraut, and kimchi to promote a healthy balance of gut bacteria. Prebiotic foods such as garlic, onions, bananas, and asparagus can also support gut health by nourishing beneficial bacteria.
- Omega-3 Fatty Acids: Include foods rich in omega-3 fatty acids, such as fatty fish (salmon, mackerel, sardines ), flaxseeds, chia seeds, and walnuts. Omega-3s have anti-inflammatory properties and may help reduce inflammation in the gut.
- Avoid Trigger Foods: Identify and avoid foods that trigger symptoms or exacerbate inflammation. Common trigger foods for individuals with UC may include spicy foods, high-fat foods, caffeine, alcohol, and foods high in refined sugars.
- Keep a Food Diary: Keep track of your dietary intake and symptoms in a food diary to identify patterns and determine which foods may be contributing to symptoms or triggering flare-ups.
Exercise can be beneficial for individuals with ulcerative colitis (UC) in several ways:
- Symptom Management: Regular exercise can help alleviate symptoms such as fatigue and stress commonly associated with UC, improving overall well-being.
- Low-Impact Options: Low-impact activities like walking, swimming, or cycling are often well-tolerated by those with UC, providing gentle movement without straining the digestive system.
- Weight Management: Exercise can help maintain a healthy weight, which is important for managing UC symptoms and overall health.
- Improved Digestion: Moderate exercise may promote better digestion, contributing to overall gut health and potentially reducing UC symptoms.
Empowering Ulcerative Colitis Management with Foodnwellness
At Foodnwellness, we understand the profound impact that nutrition can have on managing ulcerative colitis (UC) and improving overall quality of life. Our dedicated team of experienced dietitians specializes in creating personalized nutrition plans tailored to address the unique dietary needs and challenges faced by individuals living with UC.
We recognize that UC is a complex condition that requires a multifaceted approach to management, and nutrition plays a central role in supporting gut health, managing symptoms, and optimizing overall well-being. With our evidence-based strategies and compassionate care, we aim to empower individuals to take control of their health and thrive despite the challenges posed by UC.
With Foodnwellness, you’ll receive personalized nutrition guidance and ongoing support from our team of experts who are dedicated to helping you navigate the challenges of living with UC. Together, we’ll unlock the power of nutrition to elevate your digestive health, enhance your resilience, and improve your quality of life.
For personalized nutrition guidance and support tailored to your unique needs, reach out to our expert team at Foodnwellness. Let’s embark on a journey towards better digestive health and greater well-being, one nourishing meal at a time.
- Rubin, D. T., Ananthakrishnan, A. N., Siegel, C. A., Sauer, B. G., & Long, M. D. (2019). ACG Clinical Guideline: Ulcerative Colitis in Adults. American Journal of Gastroenterology, 114(3), 384–413. [doi:10.14309/ajg.0000000000000152]
- Kucharzik, T., Ellul, P., Greuter, T., Rahier, J.-F., Verstockt, B., Abreu, C., et al. (2021). ECCO guidelines on the prevention, diagnosis, and management of infections in inflammatory bowel disease. Journal of Crohn’s and Colitis, 15(8), 1274–1289. [doi:10.1093/ecco-jcc/jjaa224]
- Ungaro, R., Mehandru, S., Allen, P. B., Peyrin-Biroulet, L., & Colombel, J.-F. (2017). Ulcerative colitis. The Lancet, 389(10080), 1756–1770. [doi:10.1016/S0140-6736(16)32126-2]
- Siegel, C. A., & Melmed, G. Y. (2020). Predictors of non-adherence to biologic therapy in ulcerative colitis and Crohn’s disease. American Journal of Gastroenterology, 115(11), 1739–1742. [doi:10.14309/ajg.0000000000000770]
- Ananthakrishnan, A. N., Khalili, H., Konijeti, G. G., Higuchi, L. M., de Silva, P., Fuchs, C. S., et al. (2014). Long-term intake of dietary fat and risk of ulcerative colitis and Crohn’s disease. Gut, 63(5), 776–784. [doi:10.1136/gutjnl-2012-303304]
Let's get started with treating your condition...
At Food & Wellness we believe that every individual is different and needs special attention. We adapt our programme to your existing lifestyle and try not to change anything drastically so you can easily transition. Over a period of time we ensure results and help you restore your health.
Related Articles
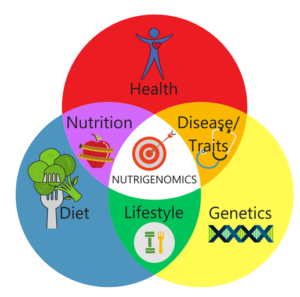
Unlocking Nutrigenomics: Exploring the Dynamic Interaction between Genes and Nutrition
Discover the fascinating world of nutrigenomics, where genes and nutrition intertwine to shape our health. Nutrigenomics explores the intricate relationship between our genetic makeup and the food we consume, offering insights into how our bodies process nutrients and respond to different dietary factors. Uncover the connections between genes, folate, caffeine, and more, as we delve into the potential of personalized nutrition for optimizing health outcomes. Join us on this enlightening journey into nutrigenomics and unlock the power of genetics for a healthier, tailored approach to wellness.

Water retention : All you need to know about it!
We’ve all heard the term “Water weight” being thrown around, but if you don’t understand what exactly it is, then those especially in the midst of a weight loss program can get quite discouraged by its contingency. Contrary to popular belief, Water retention is actually a helpful signal since it indicates the imbalance in the body.

Health or Success: What should be the priority?
How many times have you dashed out in the morning missing your breakfast because you were late for a meeting? Or how many times have you let your adolescent kid get away with store-bought junk food instead of a healthy meal because you just didn’t have the time to spend in the kitchen? Can you count the number of cups of coffee you’ve gulped in the office because you were stressed from work?